Gender Equity in Health Emergency Preparedness and Response
COVID-19 has presented us with a break in history and an opportunity to fix the structural weaknesses in our health and social systems so we can better withstand future shocks.
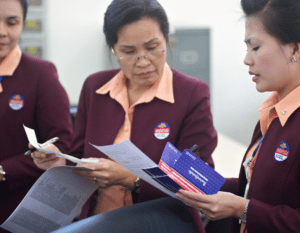
Women make up the majority of health workers, yet they hold a minority of senior decision-making roles and face unsafe working conditions, along with being paid less than their male counterparts. Additionally, the great resignation of health workers, combined with a projected shortfall of 10 million health workers prior to the pandemic, has created a significant health security issue.
A gender-responsive approach to pandemic preparedness and response would ensure that the unique needs and perspectives of women and girls are integrated into all aspects of the public health response. This includes conducting sex-disaggregated data analysis, involving women in decision-making processes, and addressing the gendered impacts of pandemics, such as increased domestic violence and unpaid care work. By prioritizing gender-responsive pandemic preparedness and response, we can promote more equitable and effective health outcomes for all members of society.

 About our work
About our work
Women in Global Health is actively working towards rebuilding a more secure and equal foundation for global health by enabling women who already deliver health to also lead it. This approach recognizes the role of women in the health workforce and the need to integrate their unique needs and perspectives into all aspects of the public health response. By prioritizing gender-responsive pandemic preparedness and response, we can ensure more equitable and effective health outcomes for all.
In December 2021, at a special session of the World Health Assembly (WHASS), WHO’s Member States established an Intergovernmental Negotiating Body (INB) to draft an international agreement to strengthen pandemic prevention, preparedness and response (referred to as the WHO CA+). Women in Global Health has worked closely with INB to strengthen gender responsiveness in both the Zero Draft (WHO CA+) and the legally-binding International Health Regulations for 194 WHO Member States.
Advocacy areas
Governance bodies, decision making bodies or advisory committees must have a 50% representation of women members, including women health workers, with a particular focus on women representatives and needs from the global south.
Women are the majority of the global health workforce (70% of all workers and 90% of frontline workers), but are only 25% of senior leaders in health resulting in decision making and planning which does not include the gender dimension of policy.
Health and care workers require fit-for-purpose Personal Protective Equipment (PPE).
A Women in Global Health survey of one thousand women from across the world found that only 14% had access to adequately fitting PPE, exposing them to increased risk of infection and also discomfort in specific use cases.
Download the Fit For Women report
Essential health services should reference maternal, neonatal and child health (MNCH) and sexual and reproductive (SRH) services.
Experience from recent outbreaks shows that family planning services can be severely compromised during emergencies. During the initial phases of the COVID-19 pandemic in 2020, approximately 70% of countries reported disruptions to these vital services – intensifying risks of unintended pregnancies and sexually transmitted infections.
Learn more about gender transformative UHC
Systems are needed to prevent and respond to cases of sexual exploitation, abuse and harassment (SEAH) and violence against women (VAW) in times of pandemic crisis.
Data on VAW, SEAH, and COVID-19 show a sharp increase. Globally, there has been a 30 per cent increase in reported cases of VAW. We call for systems in both areas, as SEAH and VAW are distinct issues.
Women health and care workers require social protection and fair and equal remuneration.
Around half of the estimated USD 3 trillion women contribute to the health sector annually is in the form of unrecognized and unpaid work. We call for fair and equal pay for all health workers, including the millions of community health workers, majority women, who were unpaid or grossly underpaid for their essential work.
Download report on women’s unpaid work in health
Financing of under-resourced services, including sexual and reproductive health services, human resources in health and mental health services.
During the Covid-19 pandemic, health spending was reallocated to the Covid-19 response and essential health services were left under or unfunded. We are calling for a requirement that financing and resourcing be readily available to ensure the continuity of essential health services which would include maternity, sexual and reproductive health services.

WGH’s Five Asks for Gender-Responsive Global Health Security
- Include women in global health security decision making structures and public discourse
- Provide health workers, most of whom are women, with safe and decent working conditions
- Recognize the value of women’s unpaid care work by including it in the formal labor market and redistributing unpaid family care equally
- Adopt a gender-sensitive approach to health security data collection/analysis and response management
- Fund women’s movements to unleash capacity to address critical gender issues
Resources

Our response to covid-19 must not be gender blind nor a gender battle

Words matter: political and gender analysis of speeches made by heads of government during the COVID-19 pandemic

Breaking the glass vial: Women at the forefront of COVID-19 vaccine

Women in leadership: Achieving an equal future in a Covid-19 world
Symptoms of a broken system: the gender gaps in COVID-19 decision-making

A gender-equal pandemic recovery needs a gender-equal health workforce

Challenges for the female academic during the COVID-19 pandemic

Enabling Women to Lead in the Health Sector: It’s Time to Fix Inequality, Not Women
Gender Dimensions of COVID-19 Pandemic
